As per reports from the Union for International Cancer Control (UICC), an estimate of 10 million deaths has been reported due to cancer across the world in 2020. In comparison, as per the Johns Hopkins data analysis by Wall Street Journal, there have been approximately 1 million deaths due to the COVID-19 pandemic in the same year. It is evident as to who is the bigger villain for humanity. Our fight against cancer is even deadlier than our fight against the COVID-19 pandemic. International Agency for Research on Cancer (IARC) reveals that 1 in 5 people develop cancer during their lifetime, and 1 in 8 men and 1 in 11 women die from the disease. These new estimates suggest that more than 50 million people are living within five years of a past cancer diagnosis.
Keeping all these intimidating and anxiety-triggering statistics in mind, any breakthroughs that happen in this fight against cancer is worth commemorating. One such recent breakthrough was made by Hadassah Cancer Research Institute at the Hadassah University Medical Center in Jerusalem. Using artificial intelligence (AI), the researchers at the institute have developed an algorithm to identify all possible harmful mutations of the TP53 gene, which are commonly found in 50 percent of tumors. The institute has reported an accuracy level of 96.5 percent. The TP53 gene provides instructions for making a protein called tumor protein p53 (or p53 or guardian of the genome). This protein acts as a tumor suppressor, which means that it regulates cell division by keeping cells from growing and dividing (proliferating) too fast or in an uncontrolled way. The most frequent cancers associated with TP53 mutations are breast cancer, bone, and soft tissue sarcomas, brain tumors and adrenocortical carcinomas (ADC). The research is being led by Dr. Shai Rosenberg of Hadassah Medical Center Cancer Research Institute and Prof Thierry Soussi, a foremost scientist of the Sorbonne University in Paris.
International Business Magazine, in support from MedCurator, the UAE-based representative of Health Plus international and marketing arm of Hadassah University Hospital, had an exclusive interaction with Dr Shai Rosenberg, MD-PhD, physician-researcher and a senior Neuro-Oncologist at Hadassah Medical Center.
AI-based Classification Model to spot cancerous mutations
Mutations in TP53 occur in roughly 42% of tumors. A germline mutation in TP53 causes the Li-Fraumeni syndrome (LFS) with a severe genetic predisposition to cancer. Classification of TP53 variants from human cancer is highly challenging. Although, the coding sequence of TP53 is small (1800 nucleotides for a 393 amino acid protein), distinguishing true driver variants from sequencing artifacts, passenger mutations and benign polymorphisms is particularly difficult as missense variants have been found at nearly every TP53 codons albeit at various frequencies with a high concentration in the 200 residues of the DNA binding domain of the protein. Multiple studies have addressed the loss of function (LOF) of p53 variants using various predictive tools, but the results are heterogeneous. In addition, although LOF prediction for hot spot variants and their strong association with a pathogenic score is quite good, it is more heterogenous for infrequent variants. As the clinical relevance of TP53 diagnostic is increasing for both somatic and germline mutations, there is a dire need for an accurate evaluation of p53 variants LOF.
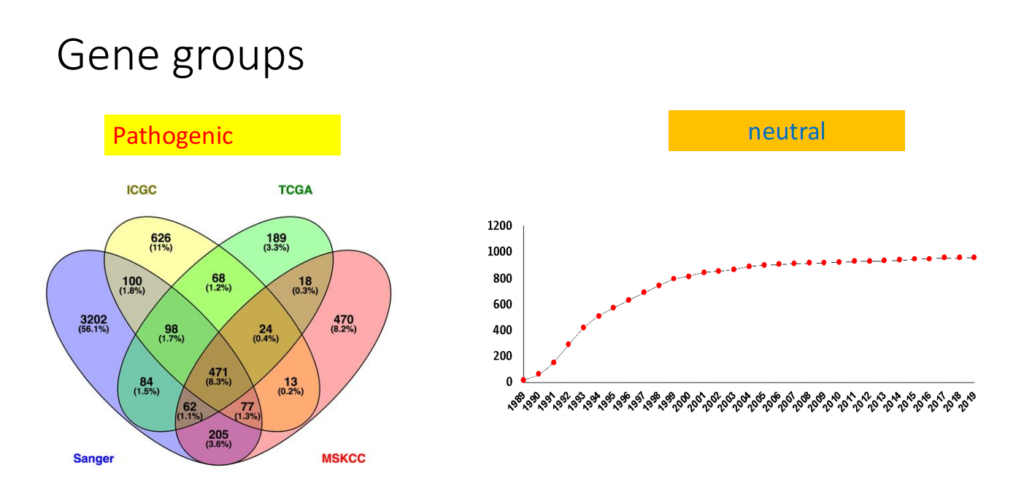
Dr Shai Rosenberg and Prof Thierry Soussi understood that there are many patients and family members carrying VUS (Variants of Unknown Significance) genes but are either not aware of it or not sure of developing cancer later in their life. Thus, the researchers noted a group of mutations based on four different independent cancer database and set up a classification between the mutations that definitely cause cancer and the ones that definitely do not. Using a computer-generated model, Dr Rosenberg and Prof Soussi are now applying it to the kind of mutations that may or may not cause cancer.
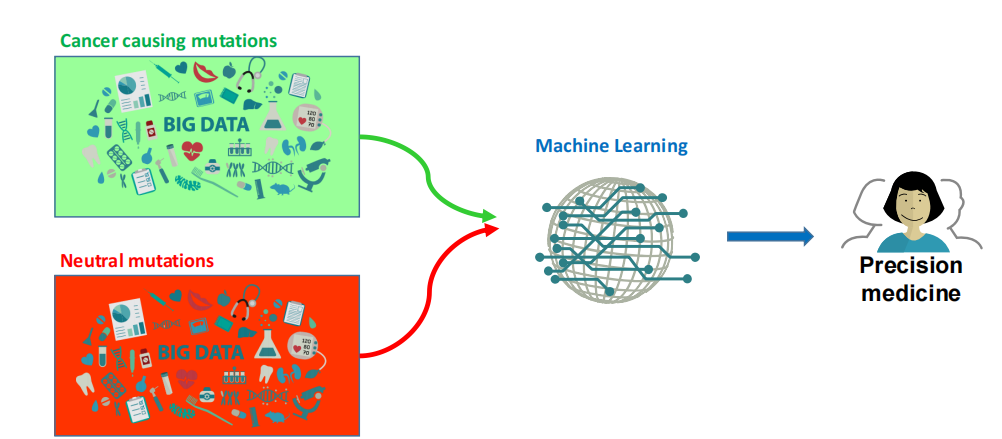
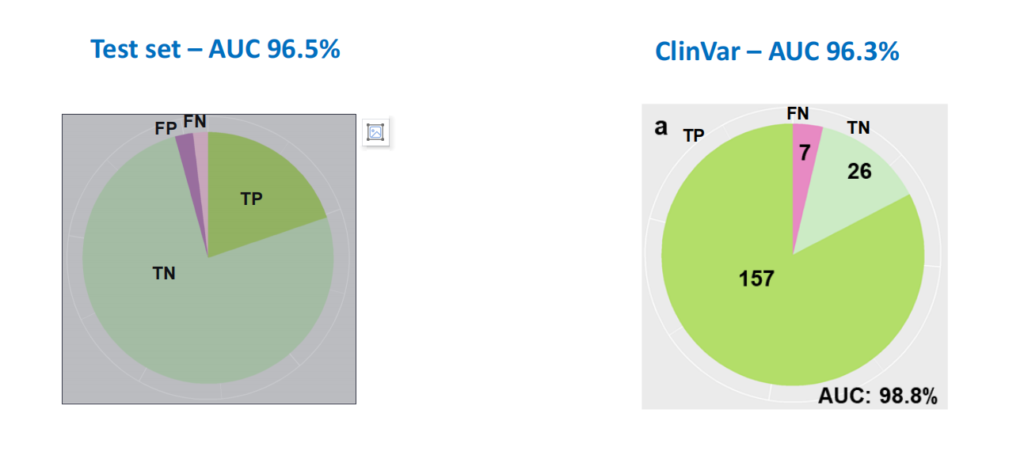
So how did this model achieve 96.5 percent accuracy? Dr. Rosenberg explains, “We trained the computer model specifically for the TP53 and not for all the genome, as is the norm in most of the ongoing research. The mutation groups were carefully defined using biological considerations and the combined computational and experimental information was considered for training. As part of the test set, we tested our model on the mutation group that we were confident about and compared the model’s predictions to the information given for the 190 mutations in the leading genetic database used for clinical application – ClinVar. We analyzed the survival data of 10,000 patients, which showed that cancer patients with mutations that the model predicts to cause cancer have shorter overall survival compared to patients with mutations considered to be neutral. The latter group had overall survival compared to patients without TP53 mutation. We performed experimental validation on 41 mutations.”
This gene-specific, AI approach can be generalized to other cancer genes and thus, contribute to more accurate genetic screening and consultation. Additionally, it can lead to more effective precision medicine for oncological patients by the creation of customized cancer treatment decision support systems that are able to identify and discern the important mutations that require treatment from the total number of somatic mutations of the tumor. The model produces a table with predictions for all possible mutations. Hadassah is already performing genomic testing for many cancer patients and they plan to apply this new model along with other contemporary models to add to the data for research and clinical validation.
Gearing up for the uphill battle against Cancer
Hadassah’s Sharett Institute of Oncology has more than 160 advanced clinical trials for eligible patients. Hadassah Cancer Research Institute (HCRI) has many cancer research laboratories. Hadassah has its own Molecular Tumor Board – a multidisciplinary team that discusses patients’ tumor genomic profiles to prescribe personalized treatment. Along with the most advanced radiotherapy equipment and protocols, Hadassah designs some of the modern electronic medical records. Its Precision Medicine and Immunotherapy approaches have showcased significant improvements in patient survival and quality of life. Hadassah has even reported cures for specific groups such as subsets of patients with metastatic Melanoma.

In his research lab, Dr Rosenberg and his eight elite research students develop novel models to quantify the effect of each mutation in cancer genes using novel deep learning algorithms and original sources of information. This is done in collaboration with many groups in the US, France, Sweden, Italy, and Israel. Dr Rosenberg is heading a program with collaborators in the Faculty of Medicine in the Hebrew University for a dual degree in medicine and computer science. This program aims to promote future physicians and researchers for medical research and development.
Revolutionizing technology for ever-evolving medicine
By 2040, the number of new cancer cases per year is expected to rise to 29.5 million and the number of cancer-related deaths to 16.4 million. Generally, cancer rates are highest in countries whose populations have the highest life expectancy, education level, and standard of living. But for some cancer types, such as cervical cancer, the reverse is true, and the incidence rate is highest in countries in which the population ranks low on these measures.
An alumnus of the Israel Institute of Technology and an expert in the subject of Neuro-Oncology, after a residency program from Hadassah – Hebrew University Medical Center in 2012, the multi-award-winning Dr Shai Rosenberg shared his insights on the upcoming fight against Cancer. “I expect that there will be more gene-targeting drugs. This in turn will lead to optimized combination therapy – to provide patients drugs that target several of the mutations identified in his/her tumor.
I anticipate more applications of immunotherapy, more drugs to enhance the immune system’s ability to fight cancer, more CAR T cells (Chimeric Antigen Receptor T cells are T cells that have been genetically engineered to produce an artificial T cell receptor for use in immunotherapy. Mostly used to treat certain blood cancers). I think that sophisticated AI algorithms will assist us more with therapy decision-making,” predicts Dr Shai Rosenberg.
Article by Ujal Nair
















